Medical
New Technology Can Break The Blood-Brain Barrier To Directly Treat Brain Tumours, Is Potent And Less Toxic, And Deserves Attention!
For brain cancer, the major obstacle to treatment is not the tumour, but the brain itself. How to break the "blood-brain barrier" and allow effective anti-cancer drugs to enter the brain to take effect has long been a key issue in brain cancer treatment. Recently, a new study has shown that a new type of pump can be implanted in brain cancer patients to safely break the blood-brain barrier and better treat brain cancer!

For brain cancer, the major obstacle to treatment is not the tumour, but the brain itself. How to break the "blood-brain barrier" and allow effective anti-cancer drugs to successfully enter the brain to take effect has long been a key issue in brain cancer treatment. Recently, a new study has shown that a new type of pump can be implanted in brain cancer patients to safely break the blood-brain barrier and better treat brain cancer!

The blood-brain barrier is a human self-protection mechanism used to prevent the core organ, the brain, from being accessed by toxins, viruses or bacteria carried in the blood. For brain cancer patients, however, the blood-brain barrier becomes a barrier to most therapeutic drugs.
Scientists have long tried various approaches such as nanoparticles, focused ultrasound, and more cutting-edge innovative chemotherapy to overcome the blood-brain barrier and treat brain tumours. Recently, neurosurgeons at Columbia University and New York-Presbyterian Hospital are taking a more direct approach to achieve that goal. They are attempting to use a fully implantable pump to deliver chemotherapy drugs directly to the brain.
A phase I clinical trial included five patients with recurrent glioblastoma. The results of this study have been published in the November issue of The Lancet Oncology. The study shows that the new implantable pump system, which effectively kills brain tumour cells, and demonstrates a safety profile for the treatment.
"This new approach has the potential to transform the treatment of many brain cancer patients, who currently have very poor survival expectations and therefore urgently need new therapies. In the future, the study will need to be tested on more patients at different stages and in different types." Dr Jeffrey Bruce, Professor of Neurosurgery at Columbia University's Vagelos College of Physicians and Surgeons and lead author of the study, said.
Typically, patients with brain cancer need to undergo surgery and have as much of the tumour removed during surgery as possible, followed by adjuvant treatment with radiotherapy and chemotherapy. Theoretically, doctors can achieve treatment by increasing the dose of chemotherapy to overcome the body's blood-brain barrier, thus allowing more drugs to enter the brain. However, when the dose is too high, the side effects are also dramatically increased and patients are often unable to tolerate the treatment.
As a result, chemotherapy is often ineffective in the face of the blood-brain barrier at doses that can be safely tolerated by patients.
"Brain cancers inevitably recur and grow after surgery," says Professor Bruce. "When they recur, there are often not many good effective treatments."
In general, patients treated for glioblastoma usually have an average survival of a little over 12 months, while once the tumour has recurred, subsequent survival can be as little as four to five months...
For the past decade, Professor Bruce and his team have been working on a pressurised pump that bypasses the blood-brain barrier and directs chemotherapy drugs to the area of the brain where the brain tumour is located.
Initial devices, including an external pump inserted through the patient's skull into the brain, could only administer a single treatment over a few days, with a not insignificant risk of infection, and the patient had to be hospitalised and hooked up to the pump device.
To overcome these limitations, Professor Bruce's team designed a new model that has no external device and allows a tiny pump to be surgically implanted in the patient's abdomen and attached to a long, thin catheter under the skin.
"We pump in the drug very slowly, about a few drops per hour, and it penetrates the brain tissue," said Professor Bruce, who has previously tested the method in a large number of animal models. "The concentration of chemotherapy drugs that assemble into a patient's brain is 1,000 times higher than if it were given intravenously or orally."
A similar implantable pump system can be used to deliver painkillers to a patient's spinal cord and keep them there for years. This pump can be refilled or emptied with a needle.
Not only that, but the wireless technology allows easy control of the pump on and off as well as the flow rate, ensuring that the drug can slowly penetrate the tumour without leaking around the catheter.
"Most drug treatments would be more effective if they could be administered over a long period of time, continuously, and without additional side effects," said Professor Bruce. "This pump could be maintained immobile for long periods of time, giving higher doses of chemotherapy directly to the area of the brain lesion without causing the serious side effects of oral or intravenous chemotherapy."
In the new study, this pump was implanted in patients with recurrent glioblastoma and filled with topotecan (which previous studies in Bruce's lab have shown may work better than the current standard drug), and a tracking agent, gadolinium, to track the distribution of the drug.
The enrolled patients received four treatments over a period of 1 month, with the pump on 2 days and off 5 days a week, 7 days a week. Patients were able to live a normal life at home and the slow pumping of the agent caused little disruption.
"The patient was walking, talking, eating and all other normal activities without even knowing if the pump was on or not." Professor Bruce said.
The study showed that none of the patients experienced any serious neurological complications with the drug, and the MRI results showed that the chemotherapy drug had successfully entered the target area within and around the tumour and that the dose was saturated.
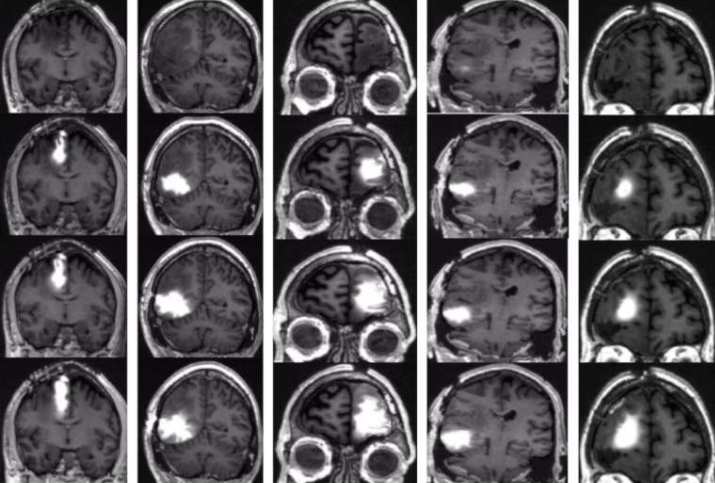
MRI scan showing that the pumped-in chemotherapy saturated the dose in and around the tumour area of the brain in each of the brain cancer patients
Although the sample size is currently small and data on the overall survival benefit for patients is not yet available, Peter Canoll, Professor of Pathology and Cell Biology at Columbia University, showed through analysis of biopsies of patients before and after treatment that chemotherapy did have a therapeutic effect, with a significant reduction in the number of otherwise active cancer cells in patients and no impact on normal brain cells.

"Tumours will be much harder to treat in brain cancer patients after initial treatment has failed, so we think this pump makes a lot of sense for patients," said Professor Bruce. "This new delivery technology, or over time, will gradually change brain cancer treatments, such as allowing the use of other, more varied types of chemotherapy - which would not otherwise be effective through systemic administration, but may be effective when administered with the pump."
-
![]()
![]() MedicalFeb 27, 2026
MedicalFeb 27, 2026Neratinib Included In NCCN Guidelines For Specific HER2-Negative Breast Cancers
-
![]()
![]() MedicalFeb 26, 2026
MedicalFeb 26, 2026New Treatment For Uroepithelial Carcinoma Receives Fda Fast Track Designation With Encouraging Initial Results
-
![]()
![]() MedicalFeb 25, 2026
MedicalFeb 25, 2026Why excimer laser can treat myopia
-
![]()
![]() MedicalFeb 24, 2026
MedicalFeb 24, 2026New Treatment For Lung Cancer Approved! Significantly Better Than Chemotherapy!
-
![]()
![]() MedicalFeb 23, 2026
MedicalFeb 23, 2026Important Target For Novel NK Immune Checkpoint Inhibitor Identified!